Genetic Disorder Lab for Newborn Screening
Raymond Vivian
Abstract
Newborn screening is a public health service that identifies infants with genetic disorders, providing early treatment and preventing symptoms from becoming worse. The lab works with genetic disease, particularly rare diseases such as metabolic disease. Using a dried filter paper blood spot, the spectrometry can identify over 30 inherited metabolic disorders in a few minutes. This will allow the pathologist to determine, based on the number of cells and other factors such as organic molecule structure, whether the baby has a potentially life-threatening disease. The correct treatment can then be given to the baby, and save their life or result in harmful effects.
Methods of Screening
The main method of screening used at labs is the Blood spot screening, sometimes referred to as the heel stick. This is where a few drops of blood from the baby’s heel are used to determine if the baby could have serious conditions. The blood is dropped into a filter paper on the card, absorbing the blood drops. The paper dries and is sent to the screening lab. There, they separate the paper by chromatography and then analyze the samples. There are around 1000 samples per year, where liquid chromatography is used for blood. Then, the screening occurs through what is called the Recommended Uniform Screening Panel, a list of disorders the Secretary of the Department of Health and Human Services (HHS) recommends for states to screen. These include organic acid conditions such as Glutaric acidemia type I, Fatty acid oxidation disorders, amino acid disorders, endocrine disorders, hemoglobin disorders, and other disorders.
Types of Spectrometry in Newborn Screenings
Tandem mass spectrometry is a powerful technology used for rapid identification of a large number of different analytes from a single sample. This is done through separating ions based on mass-to-charge ratio and measuring intensities. The molecular ions are separated by a collision chamber and mass analyzers (MS2) determine the ions mass-to-charge ratio. MS/MS can be performed on a small amount of blood and uses 2 spectrometers concurrently, eliminating prior chromatographic separation.
Single Disease Screening
Single disease screening was the original type of screening. In this kind, it was hard to add certain disorders into the list of screening as each disease needed a blood sample. It was slow and laborious, where one metabolite is analyzed in one test for one disorder, showing obvious limitations in efficiency. This style of testing also resulted in a large number of false positives and negatives, because screening results could be affected by time of blood collection and birthweight. The most common NBS programs included galactosemia, congenital adrenal cortical hyperplasia, maple syrup urine disease, homocystinuria, and cystic fibrosis. Including PKU and CH (Congenital hypothyroidism), resulted in initial success. The immediate diagnosis of PKU can prevent mental retardation in patients, and are treated using a formula that is under dietary restrictions, with dietary therapy continuing their entire lifetime. PKU was also the first screening for NBS (Newborn Screening) and achieved a lot of early success starting as early as the 1960s.
Metabolic Disorders with MS/MS Technology
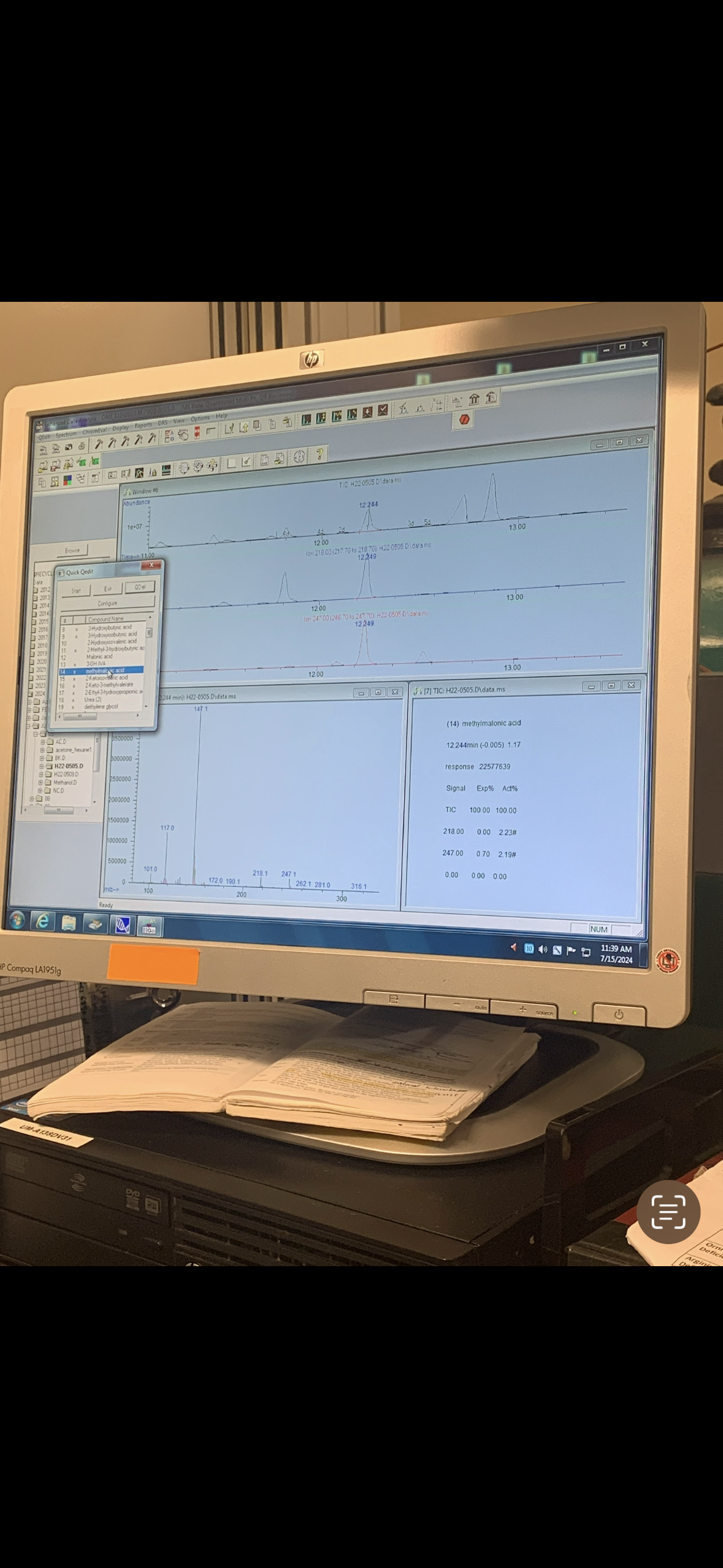
MS/MS technology for newborn screening measures two groups of analytes: amino acids and acylcarnitine species. Metabolic disorders (for MS/MS detection purposes) can be further categorized into Amino acid disorders, urea cycle disorders, organic acid disorders, and disorders of fatty acid oxidation. For new inclusion into newborn metabolic screening programs, the score had to be over 1200 for the key criteria. These criteria included clinical characteristics such as burden of disease of not treated and phenotype in the newborn, analytical characteristics like availability of the platform, and the diagnosis and treatment of condition in acute and chronic forms. For example, PKU (phenylketonuria) is one of the most commonly screened metabolic disorders. This disorder can cause seizures, developmental delay, and learning difficulties if left untreated. The figure below shows blood amino acid profile from a patient with PKU analyzed by MS/MS.
Conclusion
NBS evolved from a simple single testing screening service into a standard component of preventative health care. NBS saves millions of lives and creates bright futures for babies with rare diseases, diagnosing and treating disease within days of birth. Screening for diseases such as PKU also creates a cost-effectiveness far lower than other childhood prevention programs, creating a sustainable solution to a global problem.
References
Chen, Huey-Fen, et al. “Newborn Screening and Treatment of Phenylketonuria: Projected Health Outcomes and Cost-Effectiveness.” Children, vol. 8, no. 5, 1 May 2021, p. 381, www.mdpi.com/2227-9067/8/5/381/htm, https://doi.org/10.3390/children8050381.
Ding, Si, and Lianshu Han. “Newborn Screening for Genetic Disorders: Current Status and Prospects for the Future.” Pediatric Investigation, vol. 6, no. 4, 24 Oct. 2022, https://doi.org/10.1002/ped4.12343.
Pourfarzam, Morteza, and Fouzieh Zadhoush. “Newborn Screening for Inherited Metabolic Disorders; News and Views.” Journal of Research in Medical Sciences : The Official Journal of Isfahan University of Medical Sciences, vol. 18, no. 9, 2013, pp. 801–808, www.ncbi.nlm.nih.gov/pmc/articles/PMC3872591/. “Recommended Uniform Screening Panel | HRSA.” Www.hrsa.gov, www.hrsa.gov/advisory-committees/heritable-disorders/rusp.